MCLS shares Oral Mucositis Presentation at Multinational Association of Supportive Care in Cancer (MASCC) Annual Meeting
Beyond the Pain: Patient Insights on Oral Mucositis in Cancer Treatment, an oral poster based on patient insights gathered from the #MakeCancerLessShitty movement, was presented by MCLS ambassador Gitte Joergensen and can be viewed by clicking here.
Gitte Joergensen at MASCC
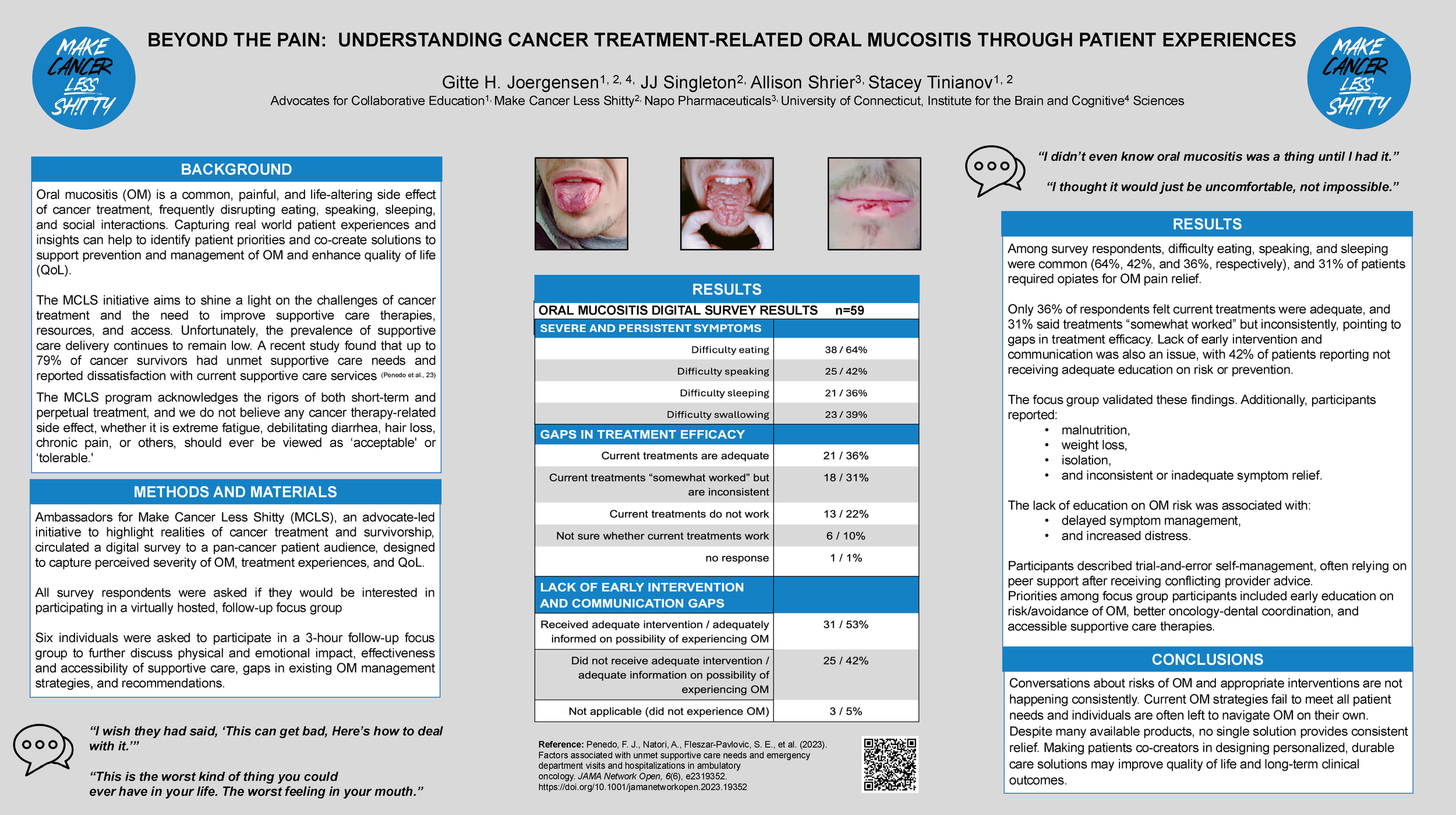
Oral mucositis is a common, painful, and life-altering side effect of cancer treatment, frequently disrupting eating, speaking, sleeping, and social interactions. Ambassadors for Make Cancer Less Shitty (MCLS), an advocate-led initiative to highlight the realities of cancer treatment and survivorship, circulated a digital survey to a pan-cancer patient audience, designed to capture perceived severity of oral mucositis, treatment experiences, and quality of life. Six individuals were asked to participate in a 3-hour follow-up focus group to further discuss physical and emotional impact, effectiveness and accessibility of supportive care, gaps in existing oral mucositis management strategies, and recommendations.
Among survey respondents, difficulty eating, speaking, and sleeping were common (64%, 42%, and 36%, respectively), and 31% of patients required opiates for oral mucositis pain relief. Only 36% of respondents felt that current treatments were adequate, and 31% said treatments “somewhat worked” but inconsistently, pointing to gaps in treatment efficacy. Lack of early intervention and communication were also issues, with 42% of patients reporting not receiving adequate education on risk or prevention.
The focus group validated all of the survey findings. Additionally, participants reported malnutrition, weight loss, isolation, and inconsistent or inadequate symptom relief. The lack of education on oral mucositis risk was associated with delayed symptom management and increased distress. Participants described trial-and-error self-management, often relying on peer support after receiving conflicting provider advice. In order to #MakeCancerLessShitty, focus group participants suggested early education on risk/avoidance of oral mucositis, better oncology-dental coordination, and accessible supportive care therapies.
As a takeaway, current oral mucositis strategies fail to meet patient needs and making patients co-creators in designing personalized, durable care solutions may improve quality of life, long-term clinical outcomes and help to #MakeCancerLessShitty.